- Benzodiazepine prescriptions and overdose mortality have increased in recent years.
- Fatal overdoses involving benzodiazepines have plateaued but not decreased among any group of Americans.
- Interventions are needed to reduce the use of benzodiazepines and to improve their safety.
- Between 1996 and 2013, the percentage of adults filling a benzodiazepine prescription increased from 4.1% to 5.6%; an annual change of 2.5%.
- The quantity of benzodiazepines dispensed in the U.S. increased from 1.1kg to 3.6kg lorazepam equivalents per 100,000 adults.
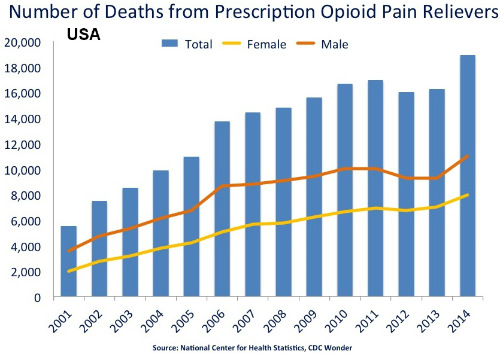
- The overdose death rate increased from 0.58 to 3.07 per 100 000 adults, with a plateau seen after 2010.
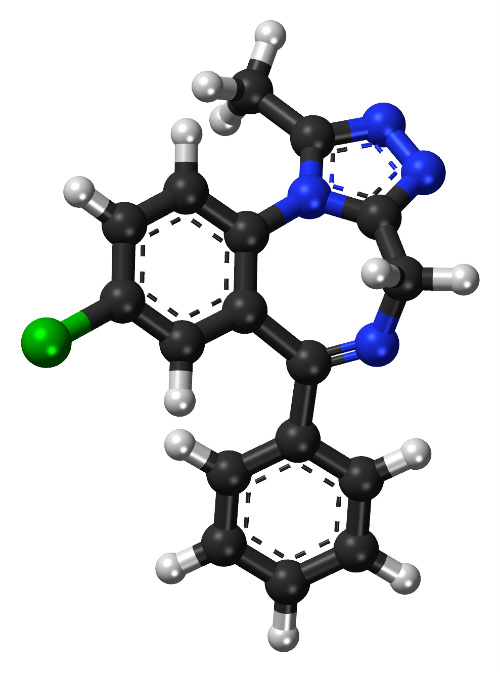
A study published recently in the American Journal of Public Health examined data from the Medical Expenditure Panel Survey and multiple-cause-of-death data from the Centers for Disease Control and Prevention (CDC) regarding overdose and death attributable to benzodiazepines. (Figure 1.)

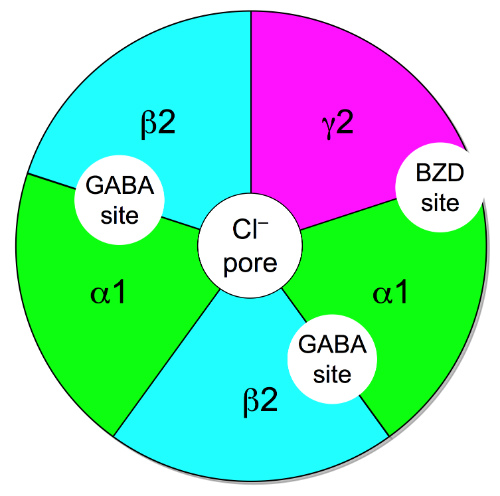
People in the U.S. consume opioid pain relievers (OPR) at a greater rate than members of any other nation. Americans consume twice as much per capita as the second ranking nation, Canada. Overprescribing of opioid pain relievers results in multiple adverse health outcomes, including overdose and death. Benzodiazepines are commonly prescribed in combination with OPR, even though this combination increases the risk for overdose. Opioid pain relievers were involved in 16,917 overdose deaths in 2011; in 31% of these deaths, benzodiazepine sedatives were also cited as contributing causes.(Figure 2.)

and are frequently overprescribed.
The Analysis
The researchers discovered that the rate of benzodiazepine overdose and death increased significantly during the study period. In the period leading to 2013, the percentage of adults filling a benzodiazepine prescription increased from 4.1% (95% confidence interval [CI] =3.8%, 4.5%) to 5.6% (95% CI=5.2%, 6.1%). The observed annual percent increase was 2.5% (95% CI = 2.1%, 3.0%), the researchers reported.
The quantity of benzodiazepines dispensed also increased during the study period, rising from 1.1kg lorazepam equivalents (95% CI=0.9, 1.2) to 3.6kg lorazepam equivalents (95% CI=3.0, 4.2) per 100,000 adults (annual percent change=9.0%; 95% CI=7.6%, 10.3%). The overdose death rate increased from 0.58 (95% CI=0.55, 0.62) to 3.07 (95% CI=2.99, 3.14) per 100,000 adults. A plateau was observed after 2010. (Figure 3.)
AJPH Recommendations
Benzodiazepine prescriptions and overdose mortality have increased considerably. Fatal overdoses involving benzodiazepines have plateaued overall; however, no evidence of decreases was found in any group. Interventions to reduce the use of benzodiazepines or improve their safety are needed.
CDC: Benzodiazepines + Opioids = ↑Deaths
A recent report in the Morbidity and Mortality Weekly Report (MMWR) a publication of the Centers for Disease Control and Prevention (CDC) was titled “Vital Signs: Variation Among States in Prescribing of Opioid Pain Relievers and Benzodiazepines—United States, 2012."
Overprescribing of opioid pain relievers (OPR) and benzodiazepines is causing an epidemic of adverse health outcomes, including fatal overdoses. Variations among the U.S. states in rates of prescribing OPR and benzodiazepines can be used to indicate areas where prescribing patterns create clinical risks for patients.
The CDC Analysis
The CDC analyzed information from an IMS Health database in order to assess the potential for improved prescribing drugs that present particular risks to patients. The CDC analysts calculated state rates and measures of variation for OPR, long-acting/extended-release (LA/ER) OPR, high-dose OPR, and benzodiazepines.
Data on prescribing in 2012 were retrieved from IMS Health's National Prescription Audit (NPA). The NPA provides estimates of the numbers of prescriptions dispensed in each state based on a sample of approximately 57,000 pharmacies. The pharmacies dispense nearly 80% of all retail prescriptions in the U.S. Prescriptions, including refills, dispensed at retail pharmacies and paid for by commercial insurance, Medicaid, Medicare, or cash were included.
The researchers found that in 2012, prescribers wrote 82.5 OPR and 37.6 benzodiazepine prescriptions per 100 patients in the U.S. Enormous interstate variations were observed in prescribing habits. Specifically, state rates varied 2.7-fold for OPR and 3.7-fold for benzodiazepines. For both OPR and benzodiazepines, rates were higher in the South, and 3 Southern states were 2 or more standard deviations above the mean. Rates for LA/ER and high-dose OPR were highest in the Northeast. Rates varied 22-fold for oxymorphone.
The Analysis
Information on local prescribing rates can alert authorities to atypical use and can prompt action. Such authorities include state and local health departments, law enforcement agencies, health-care systems, and licensure boards. States have the authority to track prescribing and dispensing and regulate medical practice within their borders. They can influence the rate of prescribing of controlled prescription drugs by various measures. These include passing regulations related to use of state prescription drug monitoring programs and the operation of pain clinics.
CDC Conclusions
Factors accounting for the regional variation remain unknown. However, the CDC analysts expressed doubt that such wide variations could be attributable to differences in the health status of the population. “High rates indicate the need to identify prescribing practices that might not appropriately balance pain relief and patient safety,” the analysts write.
State policy makers might reduce the harms associated with abuse of prescription drugs by implementing changes that will make the prescribing of these drugs more cautious and more consistent with clinical recommendations.
“Prescribers wrote 82.5 OPR prescriptions and 37.6 benzodiazepine prescriptions per 100 persons in the United States in 2012. LA/ER OPR accounted for 12.5%, and high-dose OPR accounted for 5.1% of the estimated 258.9 million OPR prescriptions written nationwide. Prescribing rates varied widely by state for all drug types. For all OPR combined, the prescribing rate in Alabama was 2.7 times the rate in Hawaii, the analysts concluded.
“The high/low ratio was greater for LA/ER OPR and high-dose OPR compared with all OPR together: for high-dose OPR, state rates ranged 4.6-fold (Delaware versus Texas), and for LA/ER OPR, state rates ranged 5.3-fold (Maine versus Texas). State rates ranged 3.7-fold (West Virginia versus Hawaii) for benzodiazepines. For both OPR and benzodiazepines, Alabama, Tennessee, and West Virginia were the 3 highest-prescribing states. Among the OPR drugs, interstate variation was greatest for oxymorphone (CV=0.72, IQ=2.50, high/low=21.9). OPR prescribing rates correlated with benzodiazepine prescribing rates (r=0.80; P<0.01),” they added.
The CDC report noted that the South region had the highest rate of prescribing OPR plus benzodiazepines. The Northeast had the highest rate for high-dose OPR and LA/ER OPR, although high rates also were observed in individual states in the South and West. In the Northeast, 17.8% of OPR prescribed were LA/ER OPR. “States in the South ranked highest for all individual opioids except for hydromorphone, fentanyl, and methadone, for which the highest rates were in Vermont, North Dakota, and Oregon, respectively,” authors noted.
The CDC reviewers reported that they were unable identify medical or surgical reason that could explain the variation in prescribing habits across the U.S. In the southern states, for instance, high prescribing rates for OPR and benzodiazepines were accompanied by high rates for other drugs including antibiotics, stimulants, and medications that are high-risk for the elderly.
“Previous studies have found that regional prescribing variation cannot be explained by variation in the prevalence of the conditions treated by these drugs. Other research indicates that wide variation in rates of surgery and hospitalization also cannot be explained by the underlying health status of the population. Wide variation in the use of medical technology, including pharmacotherapy, usually indicates a lack of consensus on the appropriateness of its use. Therefore, one possible explanation for the results of this study is the lack of consensus among health-care providers on whether and how to use OPR for chronic, noncancer pain,” the researchers concluded.
