The Centers for Disease Control and Prevention estimates that 16,000 lives are lost to opioid-related overdose in the U.S. each year, according to an article in The Washington Post. The Post article goes on to say:
“Community-based naloxone distribution programs have existed in the United States since 1996, providing the drug to more than 50,000 people and reversing more than 10,000 overdoses, according to the Centers for Disease Control and Prevention. But for years, those groups operated without much support from governments or society.”
Naloxone-distribution programs save money and they save lives. See our article on the topic here.
An opioid-related death in the ER can cost $10,000 or more. Even with the price of naloxone surging, a kit costs about $70. The literature supports the efficacy of these programs. The following is a brief literature review based on the following search term in Pubmed.com: “naloxone distribution programs.”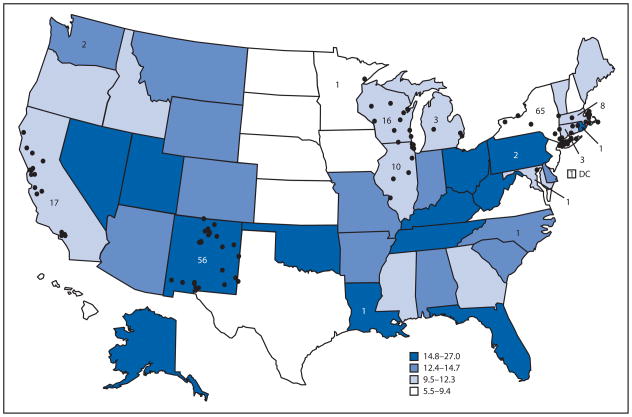
1. Opioid education and nasal naloxone rescue kits in the emergency department. Dwyer K, Walley AY, Langlois BK, Mitchell PM, Nelson KP, Cromwell J, Bernstein E. West J Emerg Med. 201516(3):381-4. PMID: 25987910.
“This is the first study to demonstrate the feasibility of ED-based opioid overdose prevention education and naloxone distribution to trained laypersons, patients and their social network. The program reached a high-risk population that commonly witnessed overdoses and that called for help and used naloxone, when available, to rescue people. While the study was retrospective with a low response rate, it provides preliminary data for larger, prospective studies of ED-based overdose prevention programs.”
2. Predictors of participant engagement and naloxone utilization in a community-based naloxone distribution program. Rowe C, Santos GM, Vittinghoff E, Wheeler E, Davidson P, Coffin PO. Addiction. 2015;110(8):1301-10. PMID: 25917125.
“Community naloxone distribution programs are capable of reaching sizeable populations of high-risk individuals and facilitating large numbers of overdose reversals. Community members most likely to engage with a naloxone program and use naloxone to reverse an overdose are active drug users.”
3. Brief overdose education is sufficient for naloxone distribution to opioid users. Behar E, Santos GM, Wheeler E, Rowe C, Coffin PO. Drug Alcohol Depend. 2015;148:209-12. PMID: 25595053.
“Opioid users seeking naloxone in San Francisco have a high level of baseline knowledge around recognizing and responding to opioid overdose and those returning for refills retain that knowledge. Brief education is sufficient to improve comfort and facility in recognizing and managing overdose.”
4. Geographic and specialty distribution of U.S. physicians trained to treat opioid use disorder. Rosenblatt RA, Andrilla CH, Catlin M, Larson EH. Ann Fam Med. 201513(1):23-6. PMID: 25583888.
“In the United States opioid use and related unintentional lethal overdoses continue to rise, particularly in rural areas. Increasing access to office-based treatment of opioid use disorder--particularly in rural America--is a promising strategy to address rising rates of opioid use disorder and unintentional lethal overdoses.”
5. What we know, and don't know, about the impact of state policy and systems-level interventions on prescription drug overdose. Haegerich TM, Paulozzi LJ, Manns BJ, Jones CM. Drug Alcohol Depend. 2014;145:34-47. PMID: 25454406.
“While important efforts are underway to affect prescriber and patient behavior, data on state policy and systems-level interventions are limited and inconsistent. Improving the evidence base is a critical need so states, regulatory agencies, and organizations can make informed choices about policies and practices that will improve prescribing and use, while protecting patient health.”
“The current evidence from nonrandomized studies suggests that bystanders (mostly opioid users) can and will use naloxone to reverse opioid overdoses when properly trained, and that this training can be done successfully through [Community-based opioid overdose prevention programs].”
7. Overdose rescues by trained and untrained participants and change in opioid use among substance-using participants in overdose education and naloxone distribution programs: a retrospective cohort study. Doe-Simkins M, Quinn E, Xuan Z, Sorensen-Alawad A, Hackman H, Ozonoff A, Walley AY. BMC Public Health. 2014;14:297. PMID: 24684801.
“Among 4926 substance users who participated in [overdose education and naloxone distribution], 373(7.6%) reported administering naloxone during an overdose rescue. We found few differences in behavior between trained and untrained overdose rescuers. Prospective studies will be needed to determine the optimal level of training and whether naloxone rescue kits can meet an over-the-counter standard. With no clear evidence of increased heroin use, this concern should not impede expansion of [overdose education and naloxone distribution] programs or policies that support them.”
8. Development and implementation of an opioid overdose prevention and response program in Toronto, Ontario. Leece PN, Hopkins S, Marshall C, Orkin A, Gassanov MA, Shahin RM. Can J Public Health. 2013;104(3):e200-4. PMID: 23823882.
“We are encouraged by the initial development and implementation experience with the naloxone program and its potential to save lives in Toronto. We have planned short-, intermediate-, and long-term process and outcome evaluations.”
9. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, Ruiz S, Ozonoff A. BMJ. 2013;346:f174. PMID: 23372174.
Opioid overdose death rates were reduced in communities where [overdose education and nasal naloxone distribution] was implemented. This study provides observational evidence that by training potential bystanders to prevent, recognize, and respond to opioid overdoses, [overdose education and nasal naloxone distribution] is an effective intervention.
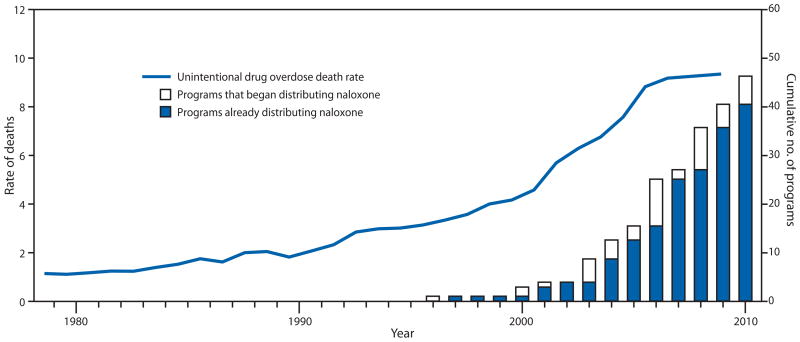
10. Community-based opioid overdose prevention programs providing naloxone - United States, 2010. Centers for Disease Control and Prevention (CDC). MMWR Morb Mortal Wkly Rep. 2012;61(6):101-5. PMID: 22337174.
“In October 2010, the Harm Reduction Coalition, a national advocacy and capacity-building organization, surveyed 50 programs known to distribute naloxone in the United States, to collect data on local program locations, naloxone distribution, and overdose reversals. This report summarizes the findings for the 48 programs that completed the survey and the 188 local programs represented by the responses. Since the first opioid overdose prevention program began distributing naloxone in 1996, the respondent programs reported training and distributing naloxone to 53,032 persons and receiving reports of 10,171 overdose reversals. Providing opioid overdose education and naloxone to persons who use drugs and to persons who might be present at an opioid overdose can help reduce opioid overdose mortality, a rapidly growing public health concern.”
