- Use the CHA2DS2-VASc score for determining which patients are at greatest risk of stroke.
- Clinicians should take an individualized approach to antithrombotic therapy.
- Strict rate control is preferred over lenient.
- Catheter ablation is a first-line option.
The most recent guideline from the American College of Cardiology on the management of atrial fibrillation (AF; Figure 1) contains important departures from previous guidelines. Among the changes are recommendations to use a more precise risk stratification scoring system, to individualize antithrombotic therapy based on shared decision-making between patient and physician, a return to strict rate control when a heart rate-control strategy is chosen, and the elevation of catheter ablation to first-line status when a rhythm control strategy is selected.
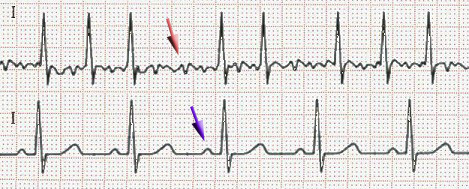
(Sources: Wikipedia/Creative Commons/By James Heilman, MD - Own work.)
Shared decision-making with respect to antithrombotic therapy for prevention of thromboembolism and preferential use of the CHA2DS2-VASc (Table) scheme (rather than CHADs) for stratification of stroke risk were 2 of the prominent changes in the 2014 American College of Cardiology/American Heart Association/Heart Rhythm Society guideline for management of atrial fibrillation (AF) compared with previous iterations.
| Table. CHA2DS2-VASc Scoring System. | |
| Risk Factor | Score |
| C (congestive heart failure) | 1 |
| H (hypertension) | 1 |
| A (age ≥75 years) | 2 |
| D (diabetes mellitus type 2) | 1 |
| S2 (prior stroke | 2 |
| V (vascular disease) | 1 |
| A (age 65 to 74 years) | 1 |
| Sc (sex [female] | 1 |
The 2014 guideline also provided recommendations for the use and selection of anticoagulants, including the non-vitamin K–antagonist anticoagulant (NOAC) agents, and targets for heart rate control.
Stroke Risk
To assess the risk of stroke in patients with nonvalvular atrial fibrillation (NVAF), defined as the absence of rheumatic mitral stenosis, mechanical or bioprosthetic heart valve, or mitral valve repair, the guideline writers recommended use of CHA2DS2-VASc score over the CHADS2 (class I recommendation). The CHA2DS2-VASc score for has a broader score range (0 to 9) and includes a larger number of risk factors compared with the CHADS2, the guideline committee noted.
“In a nationwide Danish registry from 1997 to 2008, the CHA2DS2-VASc index better discriminated stroke risk among subjects with a baseline CHADS2 score of 0 to 1 with an improved predictive ability,” the guideline authors wrote.
Individualized Approach to Antithrombotic Therapy
Risk-based antithrombotic therapy is introduced in the guideline with the following statement: “In patients with AF, antithrombotic therapy should be individualized based on shared decision-making after discussion of the absolute and [relative risks] RRs of stroke and bleeding and the patient’s values and preferences.”
Institution of antithrombotic therapy should be based on risk irrespective of the AF pattern. No antithrombotic therapy is a reasonable option for patients with a CHA2DS2-VASc score of 0 (class IIa). One of 3 options can be considered for patients with NVAF and a CHA2DS2-VASc score of 1: no antithrombotic therapy, aspirin, or oral anticoagulation (class IIb). An oral anticoagulant was recommended for prevention of stroke in patients with NVAF and CHA2DS2-VASc score ≥2 (class I). The NOACs dabigatran, rivaroxaban, and apixiban were added to warfarin (Figure 2) as preferred therapy. A NOAC was recommended for patients unable to maintain a therapeutic international normalized ratio with the use of warfarin.
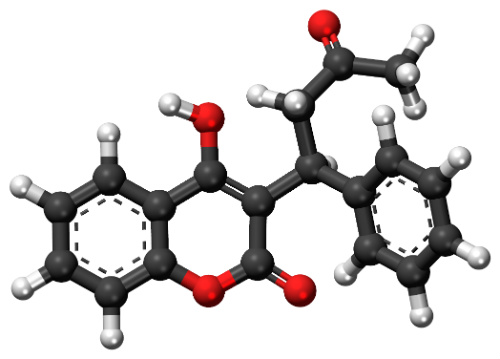
(Sources: Wikipedia/Creative Commons/By Vaccinationist.)
On major bleeding, the guideline writers concluded that apixiban had lower risk compared with warfarin, and that dabigitran and rivaroxaban were equivalent to warfarin. All 3 NOACs were deemed to have a lower risk of intracranial bleeding compared with warfarin.
Warfarin was recommended for patients with AF who have mechanical heart valves (class I), and “the target international normalized ratio (INR) intensity (2.0 to 3.0 or 2.5 to 3.5) should be based on the type and location of the prosthesis.”
Strict Rate Control is Preferable to Lenient
Strict rate control (resting heart rate [RHR] <80 bpm) is preferred over lenient rate control (RHR <110 bpm) for patients with persistent or permanent AF (class IIa). Lenient rate control may be reasonable in patients who are asymptomatic with preserved left ventricular function (class IIb).
Unless immediate rate control is required or an enteral route of administration is not available, the guideline writers recommend oral anticoagulation.
Atrioventricular nodal ablation with permanent pacing was deemed “reasonable” to control the heart rate when pharmacologic therapy is inadequate and rhythm control cannot be achieved (class IIa).
Catheter Ablation is a First-Line Option
Before initiating antiarrhythmic drug therapy, the guideline committee urged treatment of precipitating or reversible causes of AF (class I). Rhythm control should be individualized.
Catheter ablation received first-line status for the treatment of both paroxysmal and persistent AF (class IIa). According to the guideline, catheter ablation is useful for patients with symptomatic AF who are unresponsive to or intolerant to anti-arrhythmic drug therapy when rhythm control is desired (class I). Catheter ablation is reasonable in selected patients with symptomatic persistent AF prior to a trial of anti-arrhythmic drug therapy, provided that it is performed at an experienced center (class IIa).
The guideline writers cautioned that AF catheter ablation should not be performed in patients who cannot be treated with anticoagulants during and after the ablation, and AF ablation should not be performed to restore sinus rhythm with the sole intent of avoiding the need for anticoagulation (class III).
Surgical maze procedures are an option as a stand-alone for selected patients with highly symptomatic AF (class IIb) and as a concomitant procedure in patients with AF undergoing other types of cardiac surgery (class IIa).
