- The CHA2DS2-VASc is better at discriminating truly low-risk patients and finding those at high risk as well.
- In the first validation study from the EuroHeart survey, CHA2DS2-VASc had a similar C statistic to CHADS2 but improved prediction in truly low-risk patients and classified only a small proportion into the intermediate-risk category.
- the more precise the risk tool is to assess future risk of stroke, the better the chance that low-risk patients can avoid anticoagulation and that those who will benefit from anticoagulation will be identified accurately.
- The major weakness of CHADS2 is that a substantial proportion of patients (approximately 60%) are assigned a score of 1, indicating an intermediate risk of stroke, and the benefit of application of anticoagulation to this subset is uncertain.
Schemes to stratify stroke risk in atrial fibrillation (Figures 1, 2, and 3) have been used widely since the new millennium, but which scheme is best for assigning thromboembolic risk and predicting and predicting which patients may benefit from oral anticoagulation? The data demonstrate that the CHA2DS2-VASc is better at discriminating truly low-risk patients and finding those at high risk as well.
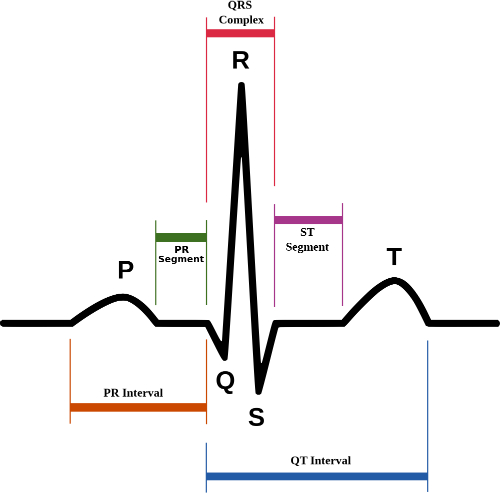
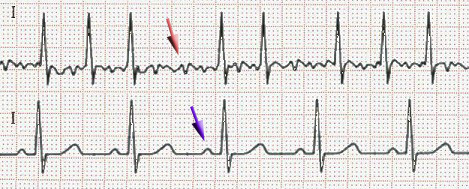
In atrial fibrillation the P waves, which represent depolarization of the top of the heart, are absent.
(Sources: Wikimedia/Creative Commons/
Created by Agateller (Anthony Atkielski), converted to svg by atom. [Public domain.])
CHADS2
The CHADS2 score was developed in 2001, and was used widely to assess the risk of stroke in patients with AF, thereby aiding clinicians in selecting AF patients who would derive benefit from anticoagulation. In 2010, a new risk score known as CHA2DS2-VASc was proposed to strengthen risk prediction by assigning points to additional risk factors not included in CHADS2: female gender, age 65 to 74 years, and vascular disease. Patients with a CHADS2 score of ≥2 are considered high risk, and are generally recommended to receive anticoagulation. The major weakness of CHADS2 is that a substantial proportion of patients (approximately 60%) are assigned a score of 1, indicating an intermediate risk of stroke, and the benefit of application of anticoagulation to this subset is uncertain.
(Sources: Wikimedia/Creative Commons CC-BY-SA-3.0 via Wikimedia Commons/
By J. Heuser (Own work) [GFDL].)
CHA2DS2-VASc
As with CHADS2, the CHA2DS2-VASc (Table) assigns a score of 0 to indicate low risk, 1 as intermediate risk, and ≥2 as high risk. In the first validation study from the EuroHeart survey, CHA2DS2-VASc had a similar C statistic to CHADS2 but improved prediction in truly low-risk patients and classified only a small proportion into the intermediate-risk category.
A validation of the two risk tools was performed by Danish researchers who used data from a national hospital registry to identify 73,538 patients with nonvalvular AF. They found that CHA2DS2-VASc was more accurate at assessing stroke risk than CHADS2.
| Table. The CHA2DS2-VASc Scoring System | |
| Risk Factor | Score |
| C (congestive heart failure) | 1 |
| H (hypertension) | 1 |
| A (age ≥75 years) | 2 |
| D (diabetes mellitus type 2) | 1 |
| S2 (prior stroke | 2 |
| V (vascular disease) | 1 |
| A (age 65 to 74 years) | 1 |
| Sc (sex [female] | 1 |
Precision
About one third of patients were defined as intermediate risk by CHADS2, but CHA2DS2-VASc had 92.7% of these patients classified as high risk. When assessing thromboembolic risk in those classified as intermediate risk via the 2 risk stratification schema, patients classified as intermediate risk by CHADS2 were found to have 4.75 thromboembolic events per 100 person-years at 1 year, compared with 2.01 for those categorized as intermediate risk by CHA2DS2-VASc. At 5 years, intermediate-risk patients as defined by CHADS2 also had more than twice the rate of thromboembolic events at 5 years compared with those classified as intermediate risk by CHA2DS2-VASc.
The proportion of patients classified as low risk of stroke was 22.3% by CHADS2, but 39.5% of these patients were intermediate risk and 21.7% were high risk using CHA2DS2-VASc, and only 8.7% of patients were truly at low risk of stroke using CHA2DS2-VASc. These results suggest that some low-risk patients by CHADS2 would actually benefit from anticoagulation.
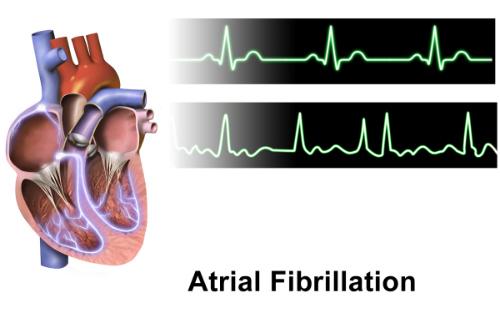
Figure 3. Normal rhythm tracing (top), atrial fibrillation (bottom).
(Sources: Wikipedia/Creative Commons/By BruceBlaus.)
Systematic Review and Meta-Analysis
A systematic review and meta-analysis of 8 studies comparing the predictive abilities of CHADS2 and CHA2DS2-VASc also determined that CHA2DS2-VASc assigned more AF patients to the high-risk group and significantly fewer (P=0.01) to the intermediate-risk group than CHADS2. “Therefore, the CHA2DS2-VASc score identifies more patients as high risk to avoid inadequate treatment,” the study authors wrote.
Further, “for the CHADS2 low-risk patients, the rate of endpoint events in the anticoagulant subgroup was significantly lower than the non-anticoagulation subgroup (0.94% vs. 1.1%), which indicates that CHADS2 stratifies some non-low-risk patients as low risk and that some CHADS2 low-risk patients can still benefit from anticoagulation.” The diversion of intermediate-risk patients to a high-risk group through use of CHA2DS2-VASc avoids the concentration of patients in the intermediate-risk group and could facilitate the selection of treatment for these patients, according to this recent study.
The value of CHA2DS2-VASc also lies in reclassification of about one fourth of intermediate-risk patients by CHADS2 into a low-risk category, a risk that is “low enough to consider withholding anticoagulant treatment,” concluded investigators who examined data from patients with AF and a CHADS2 risk score of 1 who participated in the AVERROES, ACTIVW, and ACTIVE-A trials.
This “very low-risk group” had a stroke risk of just 1% per year. “The very low-risk patients with a CHA2DS2-VASc score of 1 were men aged <65 years with either hypertension (87%), heart failure (8%), or diabetes mellitus (4%), the authors noted. “Given the risks of bleeding associated with VKA [vitamin K antagonist] treatment and the 1% per year stroke risk in patients with a CHA2DS2-VASc score of 1, we think it is unlikely that these patients will benefit from treatment with VKA therapy,” the authors noted.
Comparative Study
In a study of 2,179 AF patients who had undergone ablation, both risk scores performed exceptionally well in risk of AF recurrence, stroke, heart failure, and death at 5 years, but CHA2DS2-VASc was superior to CHADS2 in predicting AF recurrence and AF-related morbidities.
Both risk stratification schemes are easy to perform. The value of the CHA2DS2-VASc seems to lie in better discrimination of truly low-risk AF patients and in better risk stratification of those patients deemed intermediate risk by CHADS2.
