- Two studies published in Cancer reveal that uninsured and Medicaid-insured patients have worse outcomes than patients with private insurance.
- In these 2 studies, patients with private insurance had a clear survival advantage
- Based on SEER data on glioblastoma multiforme outcomes, researchers found that an uninsured patient was 14% more likely to have a shorter survival time than a patient who carried private insurance.
- A patient insured through Medicaid was 10% more likely to have a shorter survival time.
- In a study of the outcomes of men diagnosed with testicular cancer, compared with men with private insurance, uninsured men were 88% more likely to die.
- Men insured through Medicaid were 51% more likely to die of the disease.
Patients’ diagnosis of cancer and cancer survival are influenced by whether they have private insurance versus Medicare or Medicaid, according to 2 articles published recently in Cancer. Other studies have come to similar conclusions: type of insurance influences whether and for how long a patient will survive following a cancer diagnosis.
“Privately insured people with cancer were diagnosed earlier and lived longer than those who were uninsured or were covered by Medicaid, according to two recent studies,” noted an article published on NPR.org.
This finding is based on the 2 studies published recently in Cancer. One looked at patients diagnosed with testicular cancer and the other examined outcomes of patients diagnosed with glioblastoma multiforme (Figure 1). In both studies, the researchers found that patients’ date of diagnosis – within the course of the disease – and their rates of survival were both significantly influenced by whether a patient carried private insurance versus Medicaid.
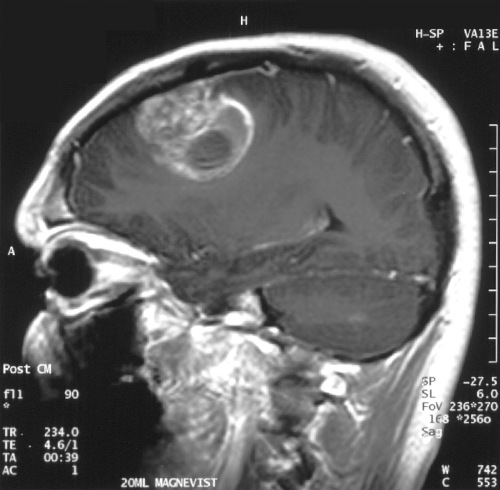
(Sources: Wikipedia/By Christaras A/Creative Commons.)
The researchers examined data from the National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) program. In the first study, the researchers analyzed SEER data on nearly 14,000 patients who were diagnosed with glioblastoma multiforme between 2007 and 2012. In the second study, researchers examined SEER data on more than 10,000 adults who were diagnosed with testicular cancer between 2007 and 2011.
"We were expecting that the uninsured would do worse than insured patients, but we didn't expect that Medicaid patients would do significantly worse than [privately insured] patients," Wuyang Yang, MD, told NPR.org. Dr. Yang is a research fellow at Johns Hopkins University School of Medicine and a co-author of the study that examined the insurance-related outcomes of patients with glioblastoma multiforme.
The glioblastoma multiforme and testicular cancers progress very differently. Glioblastoma multiforme grows and metastasizes rapidly. It is a very aggressive disease. Most patients do not survive for more than 1 year following diagnosis. The 5-year survival rate is <5%. Conversely, testicular cancer responds well to chemotherapy whether it has metastasized or not. The overall 5-year survival rate is approximately 95%.
However, regardless of the type of cancers examined in these 2 studies, patients with private insurance had a clear survival advantage.
Glioblastoma Multiforme
One of the reports published in Cancer examined the point of diagnosis in the history of the disease and rates of survival in patients with glioblastoma multiforme. The researchers found variations in insurance status among patients diagnosed with this disease. Uninsured patients and those insured through Medicaid experienced shorter survival times compared with patients who carried private insurance.
The researchers found that patients who were either uninsured or insured through Medicaid were more likely to have more advanced disease at the time of diagnosis. An uninsured patient was 14% more likely to have a shorter survival time than a patient who carried private insurance. A patient insured through Medicaid was 10% more likely to have a shorter survival time.
The authors conducted a cohort study using SEER program data from the years 2007 to 2012. Included were patients aged ≥18 years. Glioblastoma multiforme was the primary diagnosis. Patients who lacked information on their insurance status were excluded. The researchers used an accelerated failure time model to analyze survival times as coordinated with insurance status. Demographic and clinical variables were evaluated in order to account for confounding effects.
The Analysis
The cohort study included 13,665 adult patients. Of these 558 (4.1%) were uninsured, 1516 (11.1%) had Medicaid coverage, and 11,591 (84.8%) had non-Medicaid insurance. Compared with patients who were uninsured, insured patients were more likely to be older, female, white, and married. They were also found to have a smaller tumor at diagnosis.
The accelerated failure time analysis revealed that the following were independent risk factors for shorter survival among patients with glioblastoma multiforme:
- Older age (hazard ratio [HR], 1.04; P<.001)
- Male sex (HR, 1.08; P<.001)
- Large tumor size at the time of diagnosis (HR, 1.26; P<.001)
- Uninsured status (HR, 1.14; P =.018)
- Medicaid insurance (HR, 1.10; P=.006)
Conversely, the following were predictors of more positive outcomes:
- Radiotherapy (HR, 0.40; P<.001)
- Married status (HR, 0.86; P<.001)
The authors discovered an overall yearly improvement in outcomes and survival in patients with non-Medicaid insurance who were diagnosed between 2007 and 2011 (P=.015). This trend did not hold for uninsured or Medicaid-insured patients.
Germ Cell Testicular Cancer
“Patients without insurance and patients with Medicaid have an increased risk of presenting with advanced disease and dying of the disease in comparison with those who have [private] insurance, concluded the authors of this study also published recently in Cancer.
In this study of men with testicular cancer (Figure 2), uninsured patients were 26% more likely to be diagnosed after metastasis versus privately insured patients. Patients insured by Medicaid were 62% more likely be diagnosed after the disease had metastasized.
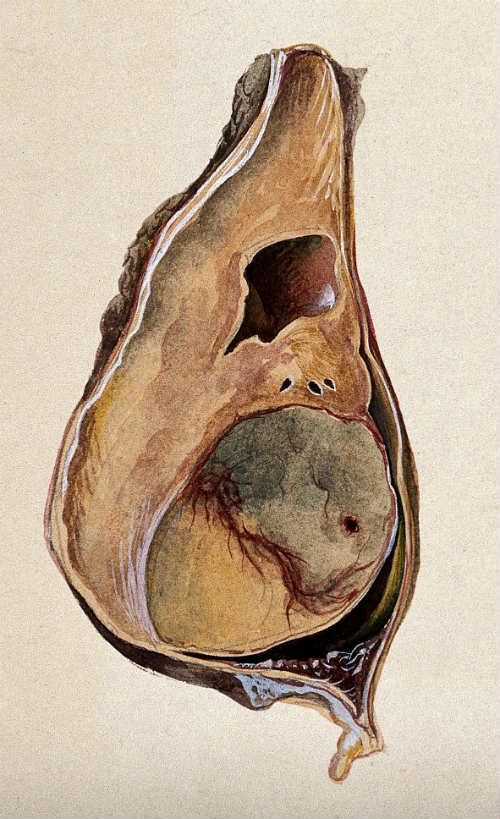
(Sources: Wikimedia Commons/Watercolor by Barbara E. Nicholson, 1958/©Wellcome Images.)
Though the Medicaid patients experienced worse outcomes than did uninsured patients, “that might be because, until recently, some of them, too, had been uninsured, the researchers say, and only enrolled in Medicaid after their cancer was diagnosed,” NPR.org reported.
Testicular cancer is particular important to study in the context of health insurance because people aged 26 to 34 years comprise the greatest proportion of the uninsured. They also have the highest incidence of the disease.
Privately insured men in the study were much more likely to survive. Compared with men with private insurance. Uninsured men were 88% more likely to die of the disease. Men insured through Medicaid were 51% more likely to die of the disease.
The Analysis
In this study too, the researchers used data from the SEER program. They identified 10,211 men diagnosed with germ-cell gonadal neoplasms between 2007 and 2011. The authors used log-binomial regression analysis to identify associations between insurance status and characteristics at diagnosis and receipt of treatment. The researchers used Cox proportional hazards regression analysis to elucidate the association between insurance status and mortality.
“Uninsured patients had an increased risk of metastatic disease at diagnosis (relative risk [RR], 1.26; 95% confidence interval [CI], 1.15-1.38) in comparison with insured patients, as did Medicaid patients (RR, 1.62; 95% CI, 1.51-1.74). Among men with metastatic disease, uninsured and Medicaid patients were more likely to be diagnosed with intermediate/poor-risk disease (RR for uninsured patients, 1.22; 95% CI, 1.04-1.44; RR for Medicaid patients, 1.39; 95% CI, 1.23-1.57) and were less likely to undergo lymph node dissection (RR for uninsured patients, 0.74; 95% CI, 0.57-0.94; RR for Medicaid patients, 0.76; 95% CI, 0.63-0.92) in comparison with insured patients. Men without insurance were more likely to die of their disease (hazard ratio [HR], 1.88; 95% CI, 1.29-2.75) in comparison with insured men, as were those with Medicaid (HR, 1.58; 95% CI, 1.16-2.15),” the authors wrote in Cancer.
Sarah C. Markt, ScD, one of the lead authors of this study, told NPR.org that she found the Medicaid results in their study striking. The findings indicate that eliminating disparities in cancer care requires more than just expanding Medicaid coverage.
"These are young men dying of a potentially curable disease. There are many opportunities for improvement here," said Dr. Markt. She is a Research Associate in Cancer Epidemiology at the Harvard T.H. Chan School of Public Health.
